Gum Disease Treatment From An Expert Periodontist
Gum Disease Treatment From An Expert Periodontist

This post explains how an expert periodontist treats gum disease using biologic dentistry principles. You’ll learn what gum disease looks like, how biologic care changes treatment, the tests that guide personalized therapy, common biologic procedures, and practical next steps for recovery and follow-up. If your gums bleed, feel sore, or your dentist recommends a specialist, this guide will help you know what to expect and how to prepare.
What Is Gum Disease And When To See A Periodontist
Stages And Common Signs
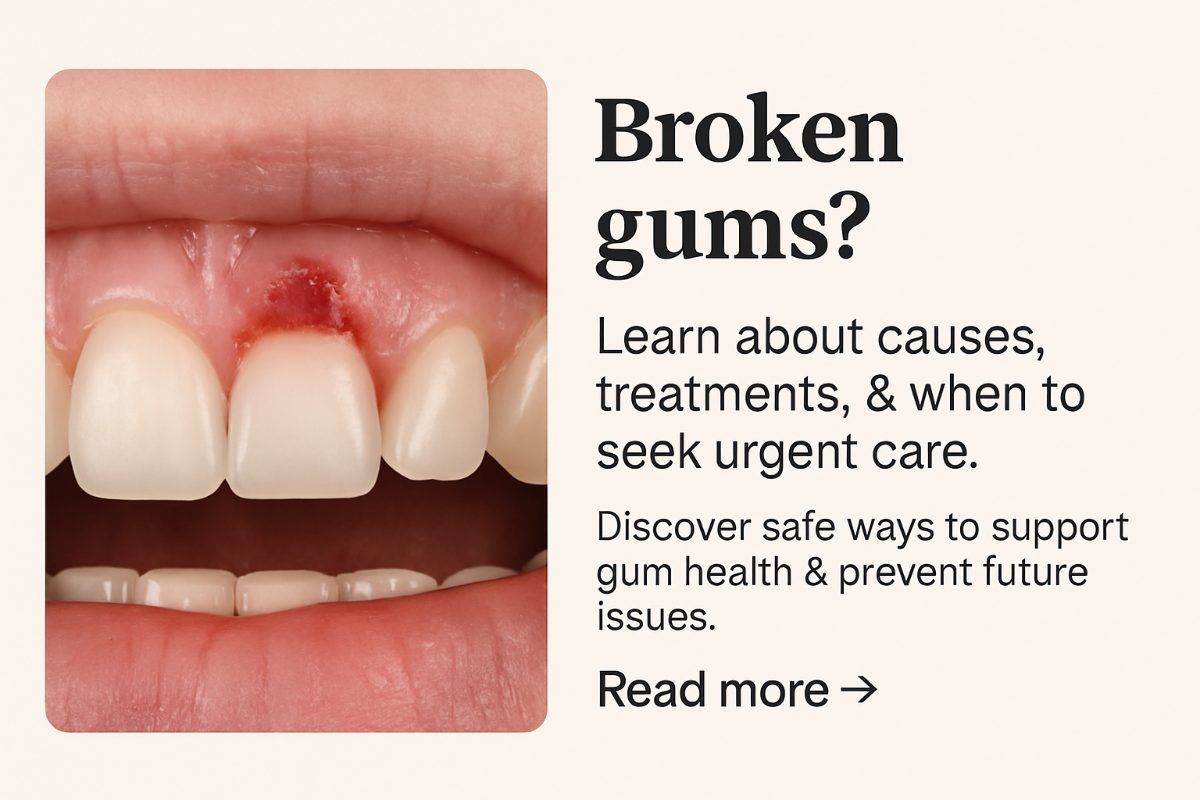
Gum disease ranges from mild gum inflammation (gingivitis) to advanced periodontitis that damages bone and soft tissue. Early warning signs include:
- Bleeding or tender gums when brushing or flossing
- Persistent bad breath or a bad taste
- Gum recession or roots showing
- Loose or shifting teeth
- Gums that stay red, swollen, or pull away from teeth
When General Dentists Refer To A Specialist
General dentists refer patients to a periodontist when problems are beyond routine care. Common reasons include persistent infection after cleaning, visible bone loss on X-rays, failed prior treatments, complex extractions, or systemic risk factors like diabetes, immune issues, or a history of cardiovascular disease. If your dentist mentions bone loss or repeated infections, see a specialist for a focused evaluation.
How Biologic Dentistry Changes Gum Disease Treatment
Biologic dentistry applies whole-body thinking to oral care. It focuses on oral-systemic health, uses biocompatible materials, and favors minimally invasive treatments. An expert periodontist who practices biologic dentistry treats more than symptoms — they look for root causes of inflammation and choose therapies that support overall health.
Core Principles
- Treat root causes of oral inflammation, not just surface infection
- Avoid toxic materials and choose biocompatible restorations
Benefits For Gum Disease Patients
Patients benefit from less invasive procedures, faster healing, and reduced reliance on systemic antibiotics. By lowering oral inflammation, biologic dentistry can also reduce long-term systemic risk and improve overall wellbeing.
Advanced Diagnostics That Guide Personalized Care
ROSA™ Screening, CBCT, And Digital Imaging
Advanced imaging maps bone, root anatomy, and airway structure. ROSA™ screening combines radiographic, oral, salivary, and airway data to give a full picture of oral-systemic health. Cone Beam CT (CBCT) and digital scans let the periodontist plan safe, precise treatment and identify bone loss or hidden infections.
OralDNA® Salivary & Microbiome Testing
OralDNA® testing identifies the specific bacteria and inflammation markers in your mouth. This lets the clinician target therapies to the organisms present, improving treatment success and reducing unnecessary antibiotics.
Biocompatibility And Airway Assessment
Biocompatibility testing helps select materials that won’t trigger sensitivities or inflammation. Airway screening checks for sleep-disordered breathing or TMJ issues that can worsen gum disease and slow healing.
Biologic Treatment Options Expert Periodontists Use
LANAP (Laser-Assisted Regeneration)
LANAP is a minimally invasive laser protocol that removes infected tissue and promotes reattachment of gums to teeth. It often means less pain, less bleeding, and faster recovery compared with traditional surgery.
Platelet-Rich Fibrin (PRF) And Regenerative Therapies
PRF uses the patient’s own blood to concentrate growth factors that speed healing and help rebuild bone and soft tissue around teeth and implants.
Ozone Therapy And Reduced Antibiotic Use
Ozone is an antimicrobial, anti-inflammatory option that can reduce bacterial load without broad antibiotics. It supports detox and healing and can be used alone or with other treatments.
Zirconia Implants, Cavitation Management, And Safe Extractions
When teeth must be removed, biologic periodontists may use zirconia implants — metal-free, biocompatible options for replacement. Cavitation management addresses infected bone areas to reduce chronic inflammation before restoration.
Material Safety And SMART Mercury Removal
Biologic care includes careful material selection and, when needed, SMART mercury amalgam removal performed under protective protocols to limit toxin exposure and support patient safety.
Recovery, Expected Outcomes, And Next Steps
Healing varies by treatment but typical timelines are:
- LANAP: reduced discomfort and improved gum health within 1–2 weeks; continued regeneration over months
- PRF and grafting: early healing in 1–2 weeks; tissue and bone maturation over 3–6 months
- Extractions and implants: initial healing in 1–2 weeks; implant integration over 3–6 months
Biologic periodontal care aims to lower oral-systemic inflammation, which can help improve sleep, energy, and chronic health conditions in some patients. Practical next steps before your visit:
- Bring recent dental X-rays and any medical records
- List current medications and supplements
- Ask about pre-visit tests like OralDNA® or ROSA™ that may speed diagnosis
Choosing An Expert In Biologic Dentistry
Look for a periodontist with formal training and certifications in biologic techniques, laser and implant training, and experience with advanced diagnostics. Board certifications, fellowship status, and documented case experience with LANAP, PRF, and zirconia implants are important markers of expertise.
Tetrahealth’s biologic-focused team — Dr. Alex Volchonok and Dr. Michele Volchonok — brings those credentials together. Their practice emphasizes ROSA™ screening, OralDNA® testing, LANAP, zirconia implants, PRF, ozone therapy, and SMART mercury removal. Tetrahealth blends advanced diagnostics and biocompatible care to treat gum disease while supporting whole-body health, with locations in Manhattan, NY and Greenwich, CT.
Schedule A Gum Disease Evaluation
To schedule an evaluation, call or book online to discuss your symptoms and share any recent X-rays or test results. At the first visit expect a focused exam, targeted diagnostics (imaging or OralDNA® testing if needed), and a clear, personalized plan that explains biologic treatment options, timelines, and next steps.